Toothache vs. TMJ Pain: Key Differences and When to See a Dentist
Key Takeaways
- Tooth and jaw pain may feel similar, but they have different causes and treatment approaches.
- Tooth pain typically arises from dental issues like decay, infection, or damage. Jaw pain often stems from joint dysfunction or muscle tension.
- Shared nerve pathways can confuse, making it difficult to determine the source of pain without professional evaluation.
- Temporomandibular joint (TMJ) disorders can mimic dental pain and often present with radiating discomfort, headaches, or clicking sounds.
- A clear understanding of symptoms, triggers, and patterns helps identify whether the pain is from the teeth or the jaw joint.
What are the most common causes of tooth and jaw pain?
Pain in the oral-facial region can be a puzzle, especially when toothaches blur into jaw pain. Understanding the root causes — no pun intended — requires looking at how dental and musculoskeletal systems overlap. Let’s break it down by source, neurological pathways, and real-life examples.
Dental Sources of Pain
Tooth pain is most commonly caused by issues directly involving the tooth structure or surrounding gum tissue. Here are the usual suspects:
- Tooth decay (caries): When enamel erodes, it exposes the inner layers of the tooth to sensitivity.
- Dental abscess: A bacterial infection deep inside the tooth can create throbbing, intense pain.
- Cracked or fractured teeth: May lead to sharp, sudden pain, especially while chewing.
- Gum disease (periodontitis): Inflammation of the gums can cause deep aches and tooth mobility.
- Post-procedural pain: After fillings, crowns, or extractions, mild pain is common during the healing process.
These pains are often localized to one tooth, are sensitive to hot/cold or pressure, and can worsen when lying down.
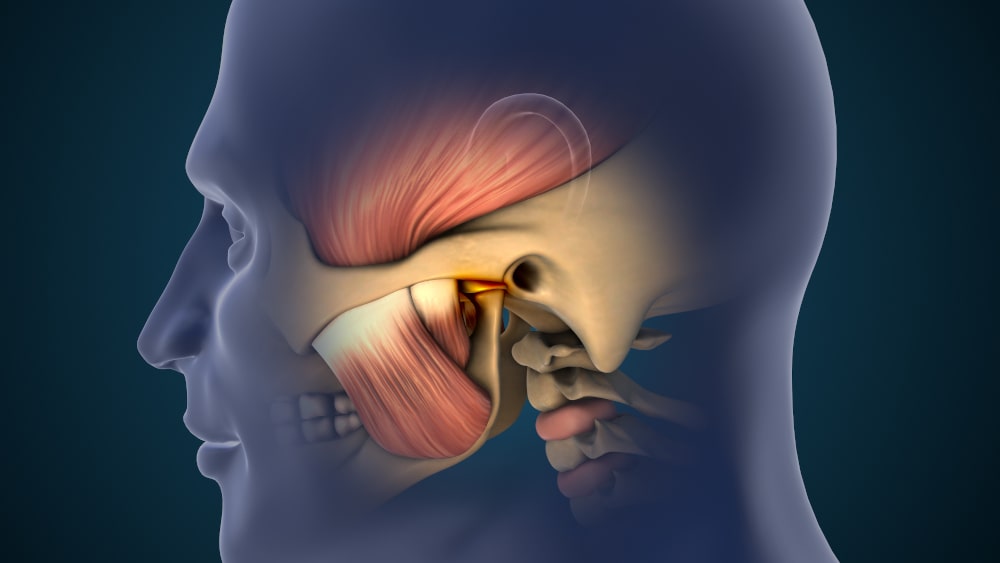
Jaw-Joint (TMJ) Sources of Pain
The temporomandibular joint (TMJ) connects the jawbone to the skull. Dysfunction in this joint or surrounding muscles can create:
- Aching facial pain
- Clicking or popping sounds when opening/closing the mouth
- Jaw locking or restricted movement
- Radiating pain to the ear, temple, or neck
- Tension headaches
Unlike tooth pain, TMJ pain is often diffuse, affects both sides, and worsens with jaw use (e.g., chewing, speaking).
Neurological Pathways and Shared Nerve Connections
Here’s where things get tricky: both the teeth and jaw are served by the trigeminal nerve, which has three branches:
- Ophthalmic (V1)
- Maxillary (V2) – supplies the upper jaw
- Mandibular (V3) – supplies the lower jaw and TMJ.
Because of this shared pathway, pain in the jaw joint can be referred to the teeth, and vice versa. This is why misdiagnosis is common and why a dental exam may sometimes require input from a TMJ specialist or neurologist.
When Pain Overlaps: A Diagnostic Challenge
Imagine this: A patient experiences sharp molar pain on the right side. No cavities, no visible issues. The discomfort worsens with chewing but isn’t sensitive to temperature. What could it be? Possibly TMJ.
Similarly, tooth pain may mimic TMJ pain by triggering reflexive jaw clenching. Chronic clenching, in turn, worsens TMJ discomfort, creating a loop.
A Side-by-Side Comparison
| Feature | Tooth Pain | Jaw (TMJ) Pain |
|---|---|---|
| Onset | Often sudden | Gradually, over time |
| Trigger | Hot/cold, sweet, pressure | Jaw movement, stress, and chewing |
| Pain Type | Sharp, throbbing | Aching, radiating, dull |
| Location | One tooth or localized area | Diffuse across the jaw, ear, and temple |
| Sounds | None | Clicking, popping during movement |
| Relief With Rest | Not usually | Often improves with jaw rest |
Research and Authoritative Sources
In the study "Temporomandibular Disorders: A Review of Current Understanding" (NIH, 2021), researchers note that TMD affects up to 10% of the population and often presents with overlapping symptoms that mimic dental problems.
Dr. Amir Guorgui, BSC, DMD, MACSD, adds: "We often see patients at Pickering Smile Centre who have tried multiple fillings or even root canals without relief — until the TMJ issue is properly identified and managed."

How do you know if you have TMJ without misdiagnosing dental problems?
Temporomandibular joint disorders are notoriously tricky. Why? Because they mimic everything from sinus issues to cavities. If you're caught between wondering whether you need a root canal or a night guard, here are the signs and self-check strategies to consider.
Red Flags That Suggest TMJ — Not a Tooth Problem
- Jaw noises: Clicking, popping, or grinding (crepitus) when opening or closing the mouth
- Limited jaw opening: Difficulty or pain when opening your mouth wide (less than 35–40 mm)
- Ear pain without infection: Particularly when there's no history of ear infection
- Worsening with jaw use: Discomfort that increases during chewing, yawning, or talking
- Waking up with pain: Jaw or temple soreness in the morning, often from clenching at night
Self-Check Cues to Try at Home
- Check range of motion: Try placing three fingers vertically between your front teeth. Can’t do it? That’s a potential TMJ sign.
- Feel your joints: Place fingers just in front of your ears and slowly open/close. Any uneven movement or crunching?
- Side-to-side test: Move your jaw left and right. Limited movement on one side suggests joint restriction.
When Symptoms Typically Worsen
TMJ pain may appear mild in the morning and worsen throughout the day with jaw use — or vice versa if you're a nighttime clencher. Tracking patterns over several days can offer insight.
According to a clinical overview in the Canadian Dental Association Journal (CDAJ), “patients with TMD often report symptoms that shift in severity and character, influenced by emotional stress, sleep quality, and posture.”
Can TMJ cause tooth pain, and why does this happen?
Yes — TMJ disorders can absolutely cause pain that feels like it’s coming from your teeth. But it’s not a dental infection — it’s a nerve confusion issue, and here’s how it works.
Mechanisms Behind TMJ-Related Tooth Pain
- Referred Pain: Because the trigeminal nerve serves both teeth and jaw, TMJ pain can travel along the same neural branches.
- Muscle Hyperactivity: TMJ disorders often cause masseter or temporalis muscles to spasm, creating pressure around teeth.
- Nerve Compression: Inflammation or joint dislocation can irritate nearby nerves, mimicking dental nerve pain.
- Bite Misalignment: TMJ dysfunction may shift how your teeth meet, causing abnormal force distribution and soreness.
- Clenching and Bruxism: TMJ stress often results in subconscious grinding, which inflames tooth ligaments.
TMJ vs. Dental Pain: Mechanism Comparison
| Mechanism | TMJ-Related Pain | True Dental Pain |
|---|---|---|
| Origin | Joint/muscle dysfunction | Tooth structure or nerve |
| Pain Nature | Diffuse, dull, pressure-like | Sharp, localized, pulsating |
| Triggered By | Stress, chewing, posture | Temperature changes, sweet foods, decay |
| Resolution | Improves with rest, jaw treatment | Requires dental intervention |
Dr. Rob Eisen explains: “The masseter muscle is one of the strongest in the body. When it's tense, it can apply up to 200 pounds of pressure on molars. That’s enough to make a healthy tooth hurt.”
What signs clearly point to a tooth infection rather than TMJ disorder?
It’s not always easy to know whether your discomfort is coming from a tooth or your jaw. But when an infection is present, it often follows a more specific path. Here’s how to tell.
Infection Symptoms to Watch For
- Swollen or bleeding gums near one tooth
- Pus discharge or a salty taste in the mouth
- Tooth discoloration or darkening
- Constant pain that worsens over time
- Fever or general malaise
- Extreme sensitivity to pressure when biting down
Step-by-Step Guide: Self-Check for a Tooth Infection
- Check the mirror: Is one tooth darker, or is it surrounded by red, inflamed gums?
- Tap test: Gently tap each tooth. Pain in one tooth more than others? That’s a clue.
- Feel your face: Any swelling, warmth, or puffiness around the cheeks or jawline?
- Note body symptoms: Fever, fatigue, or swollen lymph nodes can accompany an infection.
- Monitor pain pattern: Infections often produce constant, unrelenting pain — not just when chewing.
How does TMJ vs tooth pain differ in duration, sensation, and spread?
Identifying the source of oral-facial pain can be frustrating when there is no clear pattern. But the duration, type, and distribution of pain offer essential clues.
Key Differences in How Pain Presents
| Feature | TMJ Pain | Tooth Pain |
|---|---|---|
| Duration | Comes and goes, worsens with use | Can be constant or triggered by stimuli |
| Sensation | Dull, achy, radiating to the ear, temple, and neck | Sharp, throbbing, pulsating |
| Spread | Often affects both sides or wider areas | Usually localized to one tooth |
| Trigger Sensitivity | Triggered by jaw movement or stress | Triggered by heat, cold, sugar, and pressure |
| Pain Timing | Worse in the morning or after jaw activity | Worse when lying down or after eating |
Quick Self-Checks
- Bite Test: Gently bite down on a soft object. Sharp pain? Likely dental.
- Movement Test: Slowly open your jaw wide and move it side to side. Discomfort or restriction points to TMJ.
- Mirror Check: Look for asymmetry or swelling around the jaw joint versus the gumline.
Unilateral vs. Bilateral Pain
- TMJ: Frequently bilateral (both sides), though it may feel worse on one side.
- Tooth: Almost always unilateral and localized to a specific tooth.
What at-home strategies can safely relieve TMJ discomfort or tooth pain temporarily?
While professional evaluation is essential, temporary at-home relief can offer short-term comfort. But be careful — improper treatment may worsen symptoms.
Safe Methods for TMJ Relief
- Warm compress: Apply to the side of your face for 15–20 minutes.
- Gentle jaw exercises: Slow opening/closing, lateral movement, and resisted opening.
- Avoid chewing gum or hard foods: Give the joint time to rest.
- Relaxation techniques: Deep breathing or meditation to reduce clenching.
Safe Methods for Tooth Pain Relief
- Saltwater rinse: Helps cleanse the area and reduce inflammation.
- Cold compress (for swelling): Apply to the cheek if swelling is visible.
- Dental-safe pain relievers: Acetaminophen or ibuprofen as directed.
- Clove oil (temporary numbing): Use a cotton swab for brief relief.
When NOT to Self-Treat
- Visible swelling of the face or jaw
- Fever or chills accompanying pain
- Pain lasting more than 48 hours
- Difficulty opening the mouth or speaking clearly
Step-by-Step Guide: TMJ Relief Routine
- Apply a warm compress to the jaw joint for 20 minutes.
- Perform gentle stretches: open wide, hold, move side-to-side.
- Avoid caffeine and chewy foods today.
- Monitor pain changes — if it worsens, seek dental or medical attention.
When should you see a dentist if you're unsure whether the pain is dental or TMJ-related?
Uncertainty about the pain’s origin shouldn’t delay seeking help. Certain red flags clearly indicate the need for professional care.
Warning Signs to Watch
- Severe pain with no improvement in 24–48 hours
- Swelling in the gums, face, or jaw
- Visible pus or foul taste
- Jaw locking (open or closed)
- Pain interfering with sleep or daily function
- Persistent clicking or shifting bite
Timeline: When to Act
| Symptom | Action Needed |
|---|---|
| Pain persisting > 48 hours | Book a dental appointment |
| Fever or facial swelling | Seek immediate dental/emergency care |
| Jaw locking more than once | Schedule a TMJ evaluation |
| Radiating ear pain without infection | Consult a dentist to rule out TMJ |
What treatment options work best for TMJ issues compared to dental treatments?
TMJ disorders and dental issues require distinctly different treatment plans. Misapplying one to the other can result in persistent pain, unnecessary procedures, or even long-term joint dysfunction.
Overview of Treatment Approaches
| Treatment Type | Best for TMJ Disorders | Best for Dental Issues |
|---|---|---|
| Bite guards (night guards) | Prevent clenching, reduce joint strain | Not applicable unless bruxism affects teeth |
| Physiotherapy | Jaw exercises, posture correction, muscle release | Rarely used unless jaw muscle issues coexist |
| Stress management | Key strategy in managing chronic jaw tension | Not a primary solution |
| Anti-inflammatory therapy | NSAIDs, cold/warm compresses for joint relief | Used for abscess swelling or gum pain |
| Fillings | Not applicable | For decay or cavities |
| Root canals | Not applicable | To treat infected pulp |
TMJ-Focused Treatments
- Occlusal splints/night guards: Reduce tooth grinding and alleviate joint pressure.
- Cognitive Behavioural Therapy (CBT): Stress plays a significant role in TMJ tension.
- Manual therapy: Jaw massage, trigger point release, and physiotherapist-guided mobility work.
- Botox injections: For severe clenching and muscle spasms (used in some Canadian clinics).
Dental-Focused Treatments
- Restorative dentistry: Fillings, crowns, or bonding address physical tooth damage.
- Endodontic therapy: Root canal treatment treats deep infections within the tooth.
- Periodontal care: For gum disease, scaling and root planing are performed.
- Extractions: When a tooth is unsalvageable.
What are the key takeaways when comparing toothache vs TMJ pain?
Sorting through jaw and tooth pain isn’t always straightforward, but patterns emerge with a closer look. Here’s how to wrap up what we've explored.
Final Summary Table
| Factor | Tooth Pain | TMJ Pain |
|---|---|---|
| Pain Nature | Sharp, pulsating, pressure-sensitive | Dull, achy, spreads to temple/ear |
| Trigger | Cold, hot, sweet, pressure | Jaw movement, stress, posture |
| Location | Specific tooth | Diffuse across the face, often bilateral |
| Associated Symptoms | Swelling, fever, gum issues | Clicking, locking, and muscle fatigue |
| Duration | Constant if infected | Intermittent, worse with use |
FAQ
How can I tell if the pain is coming from a tooth or my jaw joint (TMJ)?
Tooth pain is usually sharp, localized, and triggered by cold, heat, or pressure. TMJ pain tends to be dull, aching, and radiates toward the ear, temple, or neck, often worsening with jaw movement.
Can TMJ pain feel like a toothache?
Yes. Because both areas share the trigeminal nerve, TMJ disorders can cause referred pain that feels like it's coming from the teeth, even when there's no dental issue.
Should I see a dentist if I’m unsure whether it’s a tooth or TMJ problem?
Absolutely. A dentist can assess both dental and joint-related causes of pain and refer you to a TMJ specialist if needed.
What jaw noises are signs of TMJ dysfunction?
Clicking, popping, or grinding sounds when opening or closing your mouth can indicate TMJ problems, especially if accompanied by discomfort or limited movement.
If chewing makes the pain worse, is it TMJ or a tooth issue?
If the pain is sharp and isolated to one tooth, it’s likely dental. If it's a dull ache that spreads across the jaw or worsens with repeated use, TMJ is a possible cause.
Can stress make TMJ pain worse?
Yes. Stress is a major trigger for jaw clenching and teeth grinding, which can aggravate TMJ symptoms over time.
When should I see a dentist right away?
Seek urgent care if you notice swelling, pus, fever, or severe pain that doesn’t improve within 24–48 hours — these could signal a dental infection.
How long should I wait before visiting a dentist if I’m unsure about the pain’s source?
If the pain lasts more than 48 hours or keeps returning, book an appointment. Early evaluation prevents unnecessary procedures and helps avoid worsening symptoms.